Intro (00:01):
Welcome to Health Law Talk, presented by Chehardy Sherman Williams health Law. Broken down through expert discussion, real client issues and real life experiences, breaking barriers to understanding complex healthcare issues is our job.
Conrad Meyer (00:21):
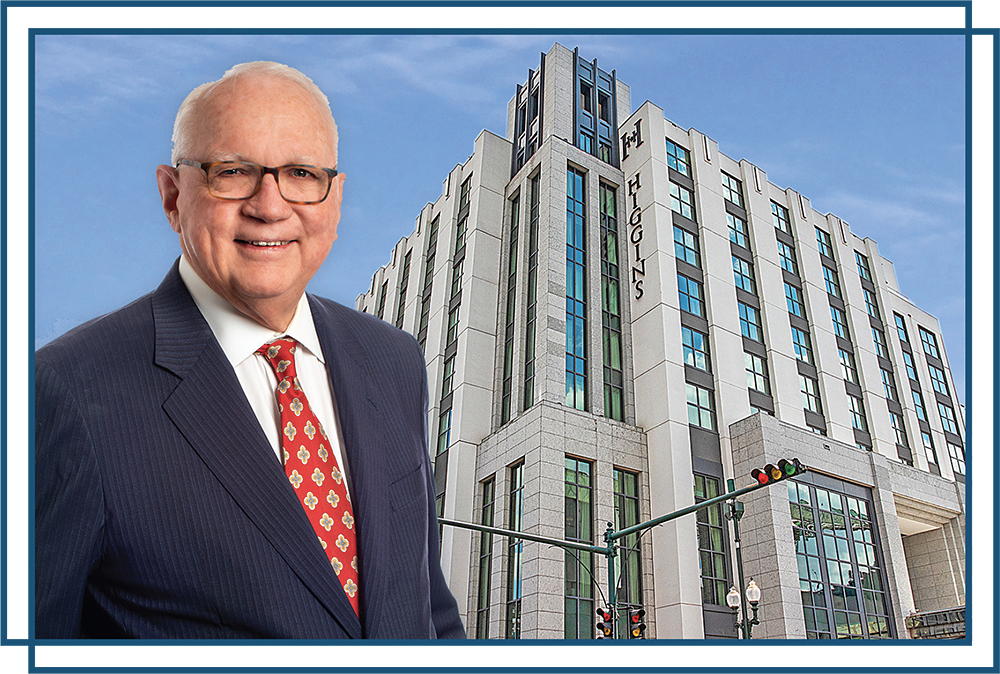
And good morning, good afternoon, or wherever you’re listening to this podcast. Welcome to another edition of Health Law Talk here at Chehardy Sherman Williams. Conrad Meyer, Rory Bellina to esteemed healthcare lawyers in the New Orleans area board certified, bringing you the greatest and greatest in health law talk. And today we have a special guest in the studio with us to help our episode out. Joe Aguilar. Joe Aguilar, a partner at HMS Valuation Partners, our first valuation speaker here. So Joe, welcome to the show. We really appreciate you coming on today. How are you?
Joe Aguilar (00:55):
Thank you. I’m doing great. Very happy to be here. This is my hometown, so it’s always great to be back in New Orleans.
Conrad Meyer (01:03):
That’s fantastic. Well, I’m glad to have you here. I know Rory is, I know we talked briefly before the show. Why don’t you tell the listeners, because we have a good provider, listener audience, what is it about, tell us a little bit about yourself. What about you do for a living? What’s your job and how does it work with healthcare? And a little bit about HMS. Sure,
Joe Aguilar (01:23):
Sure. Well, I am the managing partner of HMS Valuation partners. We’ve been around for 27 years. We actually are headquartered here out of New Orleans. Our primary work is in healthcare compliance. So we do a lot of transaction work. We do a lot of physician compensation arrangements. We do medical office timeshare real estate. So we pretty much span the spectrum both from a evaluation standpoint as well as consulting. My area of expertise has been primarily in physician compensation, advanced practice providers. I’m actually a nurse practitioner, trained in women’s health and family medicine as well. So that has brought a lot of opportunities in my work as well.
Conrad Meyer (02:10):
So a nurse practitioner and evaluation expert? That’s correct. I never heard of that combination.
Rory Bellina (02:16):
Yeah, I remember we spoke about that off air the last time we met out of town. But I’m glad you brought that up because I’ll have definitely some questions about that. So tell us about HMS, because I’m sure a lot of our listeners know what these valuation firms do. Would please tell us what your firm does?
Joe Aguilar (02:31):
Yeah, sure. So HMS is primarily focused on basically two arms of work, which is both the health system work where we’re doing a lot of the recurring regular transactions that occur every day, which could include physician employment arrangements, er call, medical directorships, you name it from that perspective. And then we also do the transaction work, which is the joint venture, the practice acquisitions and so forth. In terms of our spectrum, as I mentioned earlier, we basically take care of any transaction that comes across your desk. So we have the run of the mill real estate appraisal work, the fixed asset work, if you’re looking at an asset purchase arrangement or the physician compensation or advanced practice compensation, we also do compensation design work and then medical office timeshares. But I think one of the areas that we’re starting to see a lot more work in is in the hospital-based services arrangements. So your anesthesia, your emergency medicine work, your hospitalist work. Because as you begin to see some of those labor costs skyrocket and reimbursement less, you’re seeing these PSAs, the professional services agreements go up and that’s causing challenges for hospitals.
Conrad Meyer (03:51):
I agree. Well, I was going to ask you that. You took the words out of my mouth. This is what you’re seeing in 2024. This is a trend you’re seeing coming in for the year.
Joe Aguilar (04:01):
Exactly. So what’s happening, and I just am going to be talking on this in 2024 multiple venues, but is that hospitals are reaching a tipping point. And that tipping point has been met before, but it’s basically the same cycle. You start with A PSA at some amount, then a year later, the contractor will come back and say, well, the market dynamics are suggesting that we can’t afford this anymore. So they come back and they dip into the well again. And it’s been going on and on and on to the point where we’re starting to see, this is probably maybe about five years ago, we were starting to counsel our clients and saying, while we can support it from an FMV standpoint, is this really sustainable going forward? And at what point, what are y’all using as metrics to determine whether or not you guys should just do it on your own?
(04:51):
Because at some point in time, it gets to the point where it’s so costly that why are we losing the 20% margin to a staffing provider when we can just do it ourselves? Well, that’s a loaded question because it’s not that easy to do it yourselves either. But it’s gotten to the point where that question is being asked, and you see anesthesia coming in-house, you see emergency medicine is already coming house. You see rollups in radiology. And what we’re doing now for systems is really helping them, okay, now we’ve brought them in. What do we do now? We hand it off to our physician operation folks who are doing family medicine and cardiology and orthopedics. Well, the anesthesia scheduling and billing is a completely different animal. It’s
Conrad Meyer (05:41):
A very unique animal. And I guarantee you, you’re not going to have any physician ops people that know how to handle that
Joe Aguilar (05:46):
Well. And that’s the issue. And so even just the standpoint of understanding what you’re getting when you actually roll in that group, so are you getting a group that’s overstaffed or understaffed, overpaid or underpaid? All that matters. And we’ve done, I remember one in particular where we looked at the anesthesia group and they just were overstaffed. And so we ended up talking with the hospital system and kind of right sizing also in terms of right case mix or provider mix because we ended up using more CRNAs and we ended up saving multiples of millions on that just annually just by right-sizing the group. And then we saw an emergency medicine. I remember one in particular where the emergency medicine physicians were just workhorses, but the comp was not matching. And it was because mostly it was going to the margin or to the management fees. And so we just talked with the hospital and said, guys, you can have a win-win if you increase the comp to the physicians, and then you save on some of the margin and you just bring ’em in house. And that’s been pretty much the case. So you
Conrad Meyer (07:01):
Cut out the management fee, you appoint one doc as a medical director to let him run the schedule, and then you just play it. They know how to do it
Joe Aguilar (07:07):
Already. Absolutely, absolutely.
Rory Bellina (07:09):
And has that change been going so far? How do the providers feel about coming in-house versus working for outside company and just being that independent contractor and getting maybe the higher billables as being out of network but still having to deal with all the administrative burdens?
Joe Aguilar (07:24):
Well, I think they do give up some of the administrative burdens when they come in-house. I think it’s hit or miss. And being from New Orleans and being in New Orleans now, it’s kind of like the roo, right? If you don’t get started the right way, the gumbo isn’t going to taste good at the end, but it’s the truth. In other words, just those two examples I mentioned, when you engage the physicians, like the emergency medicine physicians who have been paid less and you say, Hey guys, we’re thinking about doing this. We’re going to roll you in and here’s, you’re going to be your new comp model. And so that’s so critical. Develop the right comp model to align incentives at the end of that, everybody’s happy. Well, we’ve seen during covid, we saw transactions where anesthesiologists were getting paid, let’s say 450,000 on average for the group. They were brought in at a hundred thousand more, let’s say five 50, 600,000. Well, it just wasn’t sustainable. And now we’re looking at the hospital saying, Hey, we just lost $50 million. Can we continue doing this? So who do they look at the physicians? And now we end up in an animosity scenario and it just doesn’t
Rory Bellina (08:39):
Work. That’s what I was thinking is that it seems to be the pendulum going back and forth on you contract this out under A PSA and they bill out of network, and then you bring them back in, and then you go back and forth. Do you see that that happens back and forth and it’s going to continue? I mean, you obviously want to find the balance, what works best for whoever your client is, whether it be the group or the hospital. But it seems to just be kind of going back and forth. I mean, we’ve seen it here locally. Definitely. We
Joe Aguilar (09:07):
Agree. I mean, in other words, what we’ll say is that we’re talking about the win for the hospital bringing in, but truthfully, the service providers have a lot to shoulder. In other words, they’re getting the exclusive agreement, but they also have the full bag to hold when it comes to, are you staffing the program? Are you making enough money to pay the physicians and so forth and so on. So it’s not an easy job. So what we are seeing is yes, it swims back and forth. And I mean, having done this now, let’s see, I started at a local firm here back in 1991. So having done this in over 30 years, you see the arc of history repeat itself? Sure,
Conrad Meyer (09:49):
Sure. See, that’s the issue. So you touched on a lot of things in a very shorter period of time, especially the dynamic. So even if it’s looking at anesthesia or if you’re looking at er, the ED department as a hospital, a former hospital guy. And so I would think, okay, my margins are getting eaten up every single year, but it’s a service. I have to have it to stay open. I have to do that. And the culture, okay, there’s a culture shift too, because I got my surgeons who are very, very nitpicky about when they want to have cases open, let’s talk about anesthesia out. And so I have to be very considerate about keeping cases open, staffing those rooms. That’s going to work. I don’t know how to do that. I’m hiring out. Well, then every single year in a contract, especially when it gets down to renewal, those docs are coming back or that group is coming back and saying, well, I want more from the kitty.
(10:44):
I want more from the kitty. I mean, it’s a natural thing. I get that. So now I’m having to say, well, I don’t have any more in the kitty. And then if I lose the docs, then I have to go get locums, which is going to cost me more. So I’m in this conundrum. And then I’m thinking to myself, okay, what’s my payer mix? And now I’m going to a value-based reimbursement on cases. How is that going to work? So how do you factor in all those factors when you sit down with your C-suite folks and say, okay, we have some serious discussions to have. How does that work?
Joe Aguilar (11:16):
Well, you said a lot.
(11:20):
No, but I think you’re right. What you said initially is that what typically drives the decision to up the ante or go back to the kitty is I need the service. And I don’t want to make it too simple, but basically they end up paying for it because they’re stuck. They’re totally stuck. Stuck. They’re stuck. And what we’re trying to say is that when you get evaluation, for instance, evaluation on the hospital-based service line like anesthesia or emergency medicine or radiology or any of those, you’re basically building an income statement that’s driven by provider compensation and staffing. And you’re basically trying to determine, okay, what’s the revenues, what’s the cost? And what’s the shortfall in order to pay an appropriate amount to all parties, physicians getting their comp and the staffing provider getting their margin. So we start there, I mean, to be honest with you, and we try to say, okay, where are they landing? Where are their revenues? Are they collecting? Because if you’re in a subsidy arrangement, you have an incentive to collect. But a lot of these anesthesiology arrangements are collections guarantees. So basically if you didn’t have a floor on the collections guarantee you were in trouble, especially during times of covid. So you look towards collections and say, are you actually doing your very best to collect? Because under a collections guarantee, there isn’t really an incentive.
Conrad Meyer (12:38):
No, you’re stuck on that. So the only other place to attack and a collections guarantee is the management fee. And then of course, you start hitting that node, everyone gets upset. There’s a lot of issues to work
Joe Aguilar (12:50):
Through. And so when we look at these things, you have to, are the FTEs being used appropriately? In other words, because management fee and margin and all those things can get rolled in by, I don’t want to say inflating, but by having too high of an FTE count that’s being rolled in. So you have to look at all that. And so we do that and we look at what’s the production? What’s the A SA units that the anesthesiology group is doing? What’s the work RVs? What’s the number of shifts being covered? And then are they appropriately using their apps versus their physicians?
Conrad Meyer (13:28):
It’s a complex analysis and you don’t just plug into a spreadsheet and say, oh, here’s the answer, right?
Joe Aguilar (13:32):
Correct. And what we say is that not every situation is going to warrant the same solution. And so I can’t just automatically say, well, once you get to this tipping point, and once you get to this per day subsidy rate, you need to reel it back in. There’s a lot of different dynamics. Has there
Rory Bellina (13:51):
Been any effect on this analysis based on no surprises going into effect, especially in our example for anesthesia and er
Joe Aguilar (13:59):
Yeah, so it impacts the reimbursement. And so yes, those are the things you have to look at and see. Because one of the things that we’ve also toed around with is the idea because from the service provider’s perspective, they’re in a volatile environment as well. So they think, how can I agree to a three-year PSA when next year my labor costs may be up and my reimbursement may be down because all the things that we’re just talking about. And so we’ve even looked at different structures with the legal and from a valuation perspective of how do you build in levers so that or triggers so that everybody’s happy, because I think that’s what, this is my personal opinion, I think that’s what the service providers are trying to do. They’re trying to get as much as they can upfront because they know they have to staff the program.
Rory Bellina (14:55):
So what do you think is better for the patient? Do you think it’s better for these services to be brought back in or based on, because the hospital is going to run better with them all being under the umbrella? Or do you think it’s better to have these outside managed by the groups that are just focusing on these special areas?
Joe Aguilar (15:14):
Boy, that’s a tough question because I think it also depends. I’m channeling my father who’s an attorney also, and it depends, was always an answer. And the reason I’m saying that is because I can see some benefits with operationally. We just talked about not everybody has the expertise in how to manage a anesthesia group or a radiology group effectively. And so bringing that in-house to a hospital doesn’t necessarily automatically indicate that it’s going to run well. And I also think that with certain specialties, it works better than others. And I think that’s also a key.
Conrad Meyer (15:53):
I think when you talk about that, and I agree with you exactly what you’re saying, larger systems have the ability to do that. They have the ability, they have the cash flow in the revenue. One of our podcasts recently, I said, how many administrators does it take to run a hospital? And I think as many as possible. As many as possible. But the smaller, I would say, private hospitals and even smaller systems, that’s not the case. So you might have to contract out those types of services because you just can’t bring in the expertise under the umbrella. You don’t have the revenue to do that. Right,
Joe Aguilar (16:27):
Right. Well, exactly. And so the working capital that’s needed and just understanding the revenue cycle management of these hospital-based specialties is just different.
Rory Bellina (16:40):
One thing that I wanted to ask you about specifically, and we’ve had a couple of podcasts on this, and one in particular, it’s a physician owned hospital that is strictly cash based. So what have you been seeing in your industry? Have you had clients approach you or systems or smaller groups look at going to a cash basis? And how does that analysis go in for your
Joe Aguilar (17:02):
Firm? Interesting. Truthfully, we haven’t done as much on that area.
Conrad Meyer (17:06):
Well, they’re unicorns. There’re not many. I mean, you have to have Medicare, Medicaid or you die, but they have some unicorns out there. Well,
Rory Bellina (17:14):
And we did a podcast with one of those, and it’s actually, it’s a local hospital here that’s strictly, I mean, he explained to us that you would go in for services and there’s a menu with all of his prices. And I didn’t know if you had had any experience with that yet or what your thoughts generally were on. Is that sustainable from HMS or from your perspective?
Joe Aguilar (17:34):
Yeah, I mean,
(17:36):
We encounter it with regards to valuation work. So right now we have several who have specialized arrangements. So concierge medicine would be one that comes that kind of work. But you also see it in some of the use Conrad’s term, the unicorn. So that highly specialized physician who may pull patients from abroad or regionally and end up doing services on a cash basis. So I think from a dynamic valuation work, it’s a little bit different because you can’t just open up the survey book and scroll your finger down and find that particular individual. But in terms of sustainability, I think it’s tough because they’re still operating under the same environment that every other hospital’s operating under, and the average individual just can’t support
Rory Bellina (18:27):
It. I mean, I like the concept of it. I really liked his model and the concept of it. But like you said, it’s been ingrained in so many people and providers of having that insurance and billing that fee for service.
Conrad Meyer (18:40):
The problem is that, just to speak to that issue is that you really have to know your market and payer mix to be able to sustain that. And the locations can be critical because you’re literally going after a very small percentage of the pie of market to sustain yourself. And so I don’t know the future of that. I, I’m looking at one of the things that I think that was important in terms of healthcare in 2024 and beyond, and I’m seeing this in provider comp and that’s why I’m pivoting. I’m sort of going along and around the barn here is compensation based on not just regular RVU metrics on value. And my issue is where are we going from what you’re seeing? In other words, I used to, and tell me this, 10%, 5% of comp used to be some sort of quality metric. It wasn’t much. It wasn’t now, now I’m seeing up to 20%, up to, in one case, 25%. And it was very difficult for the higher compensation model on a quality metric when the metrics are out of control of the physician. So patient satisfaction scores, patient surveys, and then of course you combine this with a value-based reimbursement model. What do you see down the pipe from your colleagues talking about this? How does that affect physician comp and then of course, delivery of services, what do you see?
Joe Aguilar (20:10):
Yeah, that’s a lot too.
Conrad Meyer (20:12):
I have a tendency, forgive me, but we have only have a little bit of time, so I have the tendency of trying to pack everything in, but each one of those things could be a show.
Joe Aguilar (20:21):
Yeah. Yeah. I love coming back to New Orleans, so I come as much as you want. Yes. But I think the reason I say it’s a lot is because one, we’re seeing penetration of value-based arrangements vary across the country. So our work as a firm, we do work from Alaska all the way to the keys and everywhere in between basically. So you can see a lot of variance. It’s also the chicken and the egg issue. In other words, a lot of systems are kind of hesitant to take that big step with regards to value-based compensation models when they’re still largely fee for service. And I get what you’re saying. You’re seeing some of these arrangements being in the 20, 25% quality. And yes, we completely agree. You’re seeing that. I think the key is to get alignment. And so there’s a lot of hurdles that need to be addressed before it actually becomes a successful model.
(21:16):
And so for instance, we’ve seen team models work best when you’re thinking about the use of a PP. So me as an a p for instance, some of the providers may feel like, well, wait a second, they impact my compensation. So how do we align the two together? And I do think that the quality metrics need to be meaningful because we’re no longer paying on widgets. We’re trying to pay on how well was the widget made, how effective is it? And in this case, are you creating a healthier patient in the mix? I mean, when I was practicing, we used to have to check off on the super bill. This was I guess maybe 10, 12 years ago, whether or not the patient was diabetic and did we check A1C or was it a cholesterol order? Kind of basic kind of stuff. And we’re getting there, but then you have to make sure that you have your systems in place, so your provider compensation and billing kind of all intertwined because otherwise you’re not going to be able to get enough good information’s really, really be able to determine the success.
Rory Bellina (22:29):
I know we’ve talked to some providers about this shift and how they feel about it personally. And a lot of them don’t want, they don’t want, A lot of them are very comfortable with the model of, I know I did this surgery today, I billed these codes. I know what the reimbursement is from Blue Cross, and I know I’m going to make X in two weeks, and I don’t want to rely on a patient clicking a link, taking a survey, or was my OR time under a certain threshold, or was my anesthesia time under a certain threshold?
Conrad Meyer (22:55):
Or did I like the food? I mean, did the room smell nice?
Rory Bellina (22:58):
Sure. There’s just, well, the swarms so many variables. I think that it’s a shift, like you said, everything has been, and it’s a slow shift. And I don’t know if providers really want that shift new.
Joe Aguilar (23:10):
Well, I think the newness is always scary. And so usually when we are talking about compensation design changes, we really try to start with kind of a crosswalk. So don’t change anything. Let’s just do it mathematically so that we can show you what does it look like. And I think that’s an important first step to showing physicians. If we started a year where we just tracked you, we kept your, the same as it always has been, but we track all these metrics and we say, okay, if we would’ve flipped the switch, here’s the way your comp would’ve rolled out, and you’re going to have winners and losers. So you’re going to have those who are happy and those are not. But I mean, getting to your other point, in other words, I know we’re talking patient satisfaction and that’s really tough, but even just the act of improving one’s care.
(24:00):
So in other words, now the A PP had comes on, I mean, I had many patients who would tell me, I work 40 hours plus a week. I have an elder at home that I’m caring for. Yes, I know I’m my A one C’S seven or an eight, but I just can’t find the time to exercise or I can’t find the time to do these things. And truthfully, there were very real scenarios that were barriers, and it’s like, well, how do I get judged on that when some of the factors are outside of my control? And I mean, the other way is to say, okay, don’t judge on the A1C, but judge whether or not I ordered tests. Well then I don’t know if that’s, you can just click the box, then it’s clicking the box. So it’s a really tough thing to get right.
Conrad Meyer (24:57):
Well, I think Medicare is going to drive that bus too. So I mean, they’re looking to move to episodic payment. And so if they do it, then all of the big boy commercial payers can do the same. So is the tidal wave coming? I mean, do you see that, I mean from what you’re even, I’m talking at the A HLA events. You’re talking to policymakers maybe here locally and even really in DC or hearing from CMS folks. Do you see the tidal wave coming?
Joe Aguilar (25:24):
I would like to see a tidal wave of quality come. My worry is that it feels the same as when we had staff model HMOs 30 years ago, and we were trying to bring things in-house all under one roof so that we can control the cost and control the quality. And then that didn’t work. So I don’t know if we’ve got all folks moving in the same direction. You need the payers, you need the providers. And it’s really tough to get everybody,
Conrad Meyer (25:58):
There’s been a distrust for that for years, decades. I mean, that’s the problem.
Joe Aguilar (26:02):
That’s the real problem. Now look, you got Optum, they acquired so many last year physicians, they’re up to 20, 30,000 in terms of providers. That’s huge. I do think the concept works. In other words, having a system, a true system where you have providers under one roof, you may have the payers under that same roof and you’re better able to manage and control cost. But I don’t know if it’s going to be a wave. There’s a few more steps that need to fall before I can say
Conrad Meyer (26:35):
That. I don’t disagree with that, but I just was curious what your thoughts were. I have sat in meetings at a board level for iPASS under in an MA program, and I could tell you the management of the care is, so the drive, the data dive down in the drive is down to the prescription, the amount you write, the drugs you write, I mean, it is that minute. And so I wonder sometimes, is there a corporate practice of medicine issue? I mean, are we walking a thin line where you just mentioned Optum, I guarantee you over the 20 or 30,000 physicians there, and this is why I asked, how many administrators do you need? How many VPs of whatever do you need in a payer to manage and drill down to the data for 20 or 30,000 physicians to, like you said, control and manage? Are we walking a fine line? I mean, are we allowing docs to actually freely practice? I mean, what are your thoughts on that?
Joe Aguilar (27:50):
Yeah. Well, it comes to mind like the CVS care, that’s not doctors, but it’s apps where you have an algorithm. I mean, friends of mine who would, and I don’t know if it’s the same now, but years ago when you would sign up and work at one of these MinuteClinics or one of the, I’m not saying MinuteClinic per se, but one of those, you were restricted to only diagnose a specific set of diagnoses. And if you diagnosed that particular ailment, you were only given a select few prescriptions that you can choose from. Now, I mean, to a certain degree, you can say, well, that’s algorithmic and that’s evidence-based practice. And these certain things should drive what you do. I think that it’s in reality, when you’re actually seeing the, I mean, that may work for a sinusitis or a UTI or a sprained ankle, but when you’re dealing with more complex folks, it’s not going to work.
(28:50):
I mean, perfectly. I had a very healthy 50-year-old executive. She had just come back from Mexico on vacation. She was about to go to another business trip. She came in to get some refills, and every provider knows this. It’s as soon as you hold the handle on the doorway to get out the door, you always get that, by the way, question. And she said, well, by the way, when I was running on the beach in Cancun, I’d get heartburn. So can you give me some Prilosec or some medicine from a heartburn? And I said, well, tell me more about this. And what she described was pretty classic angina in women Here you’re looking at her. And she looked fine. Yeah, fine. So if I’m looking at an algorithm, I’m probably think, well, she’s fine. And sure enough, she had 99% blockage.
Conrad Meyer (29:46):
Oh
Joe Aguilar (29:46):
My God. And so it’s an art form. And so I don’t think it’s so much an art form that we can’t have some parameters to help with cost, but we need to leave a little bit of that decision making still in the patient room.
Conrad Meyer (30:04):
I mean, I agree with that. My concern is, especially now with your chat GT or ai, because I mean AI is being talked about in healthcare, mean all over the place, especially with big data. And we could give into the whole weeds and that, but are we going to sit, just have a terminal, hire somebody, whether it’s an A PP or even an RN who just gets all these little machines and gets all the data in. And Jarvis is going to say, okay, nurse, give her this, give her this, give her
Joe Aguilar (30:31):
This. I have another story. So I would say no,
Conrad Meyer (30:37):
Because an art form, I agree with you.
Joe Aguilar (30:38):
Well, okay, I just had this conversation just the other day with, and primary care is what I did. And primary care is number one thing about primary care in my mind is it’s relationships. So I had a very strong farmer in Wisconsin where I had to practice. This fellow was, I think he was in his high seventies. He came in with what he called an infection on his arm. He said, Hey, they called me Dr. Joe, can you go ahead and take care of this? Give me some SAV or something. And I said, well, you know what? This looks a little different. Lemme cut it out and lemme see. Well, it turned out to be basal cell carcinoma. He and I talked about his corn farms and other things that he liked, the Wisconsin badgers and all the fun things while I was doing the procedure with him.
(31:24):
And well, he felt comfortable enough coming back a week later to tell me what really was going on. Well, he ended up having stage four penile cancer. And when you’re at that stage, he had visibly enlarged inguinal lymph nodes to the size of softballs. And I called the UW Madison urology team, and he told me, he says, I doubt what you’re seeing because I’ve only seen one. And I said, well, I think you’re about to see number two. And sure enough, that’s what he had. But whenever I have residents or medical students that I’ve been able to come across and talk to, that to me is a telling story in primary care. Because that fellow had this issue going on for years. And it wasn’t until I took care of what he called an infection, which was incredibly minor and sat and talked with him about that.
Conrad Meyer (32:18):
He felt comfortable
Joe Aguilar (32:19):
That he felt comfortable, right? Because it was a sensitive issue. And here he came. If he would’ve had a relationship like that with somebody earlier, potentially we’d have got caught it sooner. So I think that’s, you can’t algorithm that.
Conrad Meyer (32:32):
I pray that it doesn’t come to that.
Joe Aguilar (32:34):
I pray it doesn’t come to that. Yeah, Jarvis can’t solve that.
Conrad Meyer (32:37):
Jarvis can’t solve that problem. Right? I’m with you. But are
Rory Bellina (32:39):
You seeing restrictions being put in place by some of your hospital clients on those metrics for patient encounters, patient times? Because all that has to be measured to calculate. So swing the pendulum back in your example of meeting with that patient, that’s not another encounter that you got to bill for. That’s not another encounter that if you worked for a hospital, they would be able to bill for, and you sent that case out to urology. So all of those things hospitals are looking at as well, that was a waste of our time because they didn’t financially benefit from it. So what are your thoughts on that?
Joe Aguilar (33:12):
Yeah, I mean I think that gets down to the comp design that gets down to compensation expectations by providers, all of that. So in other words, you also said a lot, so I want to make sure I hit on all the things you said. I think that with respect to compensation or style of practice, for instance, sure. If you are going to want to have that style where you spend more time and you have less work RVU and you have less collections, it’s going to impact compensation. And that’s a reality. I think you have to make sure that you are building that in. I guess with respect to, I don’t want to say, yeah, you have to build it in with respect to the money and whether or not the finances are there to support what you’re doing. But it’s still, I think that’s where if you work as a system and you’re looking at things collectively, and hopefully it’s a little bit tougher in this instance, I have to send them completely out. It’s not that tough. If we’re talking about cholecystectomy, let’s say, where I’m setting that patient within my hospital system, let’s say. It’s easier to kind of try to manage that, but ultimately you want to make sure that you do the right thing for the patient from that perspective.
Conrad Meyer (34:35):
One thing, I’m going to switch gears because we’re seen with physician comp, but one thing I want to ask you, and we see it a lot here, is in employment contracts, there’s always a clause, and I’ve seen it consistently now that hospitals will refuse or will cap compensation on FMV to avoid any kickback issues or stark issues. Usually it’s any kickback issues. So I don’t know if you saw the case recently, that case you and I talked about the $310 million DOJ settlement with a system. What state was it in? Was it St. Louis?
Rory Bellina (35:14):
I believe it was somewhere in the Midwest. Midwest, I believe
Conrad Meyer (35:16):
Midwest. I can’t remember what, but it was basically an issue where they overcompensated the docks and they got hit with the DOJ whistleblower action and settled for 310 million on an over comp. And usually every time I get, and the reason I’m bringing this up is because we get it on the hospital side, we usually get on the provider side where the docs would say, I don’t want that cap in place. I don’t want that. And usually when I look at the MGMA numbers for the specialty and the given area for that specific situation, the comp that these hospitals are offering the doc, it’s running around the median range. And so I said, look, you have a long way to go before you hit the 90%. I don’t know if they’re ever going to get you there. I mean, you’re talking maybe 10 God knows how many years. So I wouldn’t worry about it. But my question to you is, how do you advise facilities on the cap? In other words, I know you’re asked, sometimes we think it’s just a thing they throw in there so they don’t have to pay ’em anymore. But is that a real issue for you? Is that something real and tangible, and how does that play out in your world?
Joe Aguilar (36:25):
Yeah, so it’s very real and we see it quite often. I’ve seen it also described as a soft cap, and basically it’s a speed bump. It’s basically a means for the system to be able to double check and make sure that everything is still compliant. What I think happens in day-to-day life is that you may have a physician who is getting paid for their clinical services and then they add an A PP, so then they get paid a PP supervision, and then there may be some graduate medical education. So they get paid for that. And then you get all these stackable elements that start to add up. And if you’re not careful, I mean they can get out of alignment. And because of all the moving parts and all the people that are involved, I think that what we see is that soft cap as a means to just make sure that there’s actually something in finance that says, if it’s over this number, hey, let’s just take a look at it. I think that, well, lemme,
Conrad Meyer (37:27):
What’s that percentage in your head? We use MG MAA lot, and I, there’s others out there too, but what’s your red zone? Red zone area for percentage of total comp given using an MGMA standard? Is it 85? 90 95? What, in your mind, where does that red zone hit? Well see,
Joe Aguilar (37:48):
It’s interesting. We do valuations for our clients when they are in excess of the norms. So
Conrad Meyer (37:56):
Beyond way beyond that,
Joe Aguilar (37:57):
We’re way beyond that. But it depends. So in other words, if you look at the recent guidance in the last two years ago, CMS was very clear in the sense that they don’t want to put a bright line. It’s not if you go over this number, you’re outside of FMV, because if you are also over just even the median, depending on your production, they could argue that that’s also outside of FMV. It depends, well,
Conrad Meyer (38:21):
How many DOJ suits it have to bring for that? I mean, it would be staggering.
Joe Aguilar (38:25):
Yeah. So I think the point that you’re making is that I would say from a cap standpoint, what we like to say is that if you’re adding work, so where the cap really gets to be, I don’t want to say a problem, but it does present an issue, is if, let’s say you’re a three general surgery group for a hospital, and each of you guys are taking 122 days of call and somebody leaves, and all of a sudden now you’re having to take another 60 days of call, well, now you’re bumping up the cap and then the cap presents a problem, and then finance can’t pay you, compensation’s delayed. Now you got to go see a guy named Joe. That happens all the time, and that’s what gets people annoyed. So in my mind, I think you could argue that for those types of situations when there’s actual work that can be documented, like another call shift that’s being done, or you’ve added an administrative role to this particular physician or something that you could potentially move the needle further. That’s a good point. So you could add to the cap from that standpoint.
Rory Bellina (39:34):
On that same topic, what do you do when you run into a system that is able to get or wants to employ that rockstar double board certified specialist who is going to generate a ton of revenue and refer a ton of cases, but they’re worth it and their training deserves extra comp. But you’re outside of MGMA, you’re outside of all the numbers. What do you do in that case? Because fair market value at that point doesn’t really mean anything because there is no fair market value for that 1% surgeon that goodwill, right.
Joe Aguilar (40:06):
Well, I mean, I think I have been doing this along with many other, I guess a few others for 30 years that we’ve kind of built the model. And this is across a few other firms as well. It’s not just us. But so what I mean by that is it’s not without kind of some guidance. So when I think about what you’re saying is that there are those rock stars, there are those unique folks who are first in the world to do a particular case or working on revolutionizing research or what have you. So I think you have to go beyond the surveys. And so that’s the other thing that we’ve been very happy with with regards to CM S’S commentary, is that the surveys are what they consider the starting point. It’s not the end point. So we don’t look at 90th percentile as the end.
(40:54):
I can tell you I’ve delivered many in the last month that are multiples of the 90th. And it’s because that’s who we get called, that’s who pays us to do the work for that. And I think that, just to give you more concrete answer is that, so for instance, if you do have a subspecialty that’s highly compensated, maybe doesn’t have as many folks in the sample size, we’ll do internal surveys ourselves with similar positioned physicians across the country, whether that’s in an academic setting or whether it’s in a non-academic setting. And we’ll do our own interviews and we’ll try to assess, well, what is the market for this physician when there’s only a hundred of ’em?
Conrad Meyer (41:38):
Alright, I got to good one for you. Here we go. Okay. On your FMV opinion, when you do it for the facility or whoever you’re doing, yeah. Ever been challenged by one by DOJ?
Joe Aguilar (41:47):
No, we haven’t. Thankfully You didn’t
Conrad Meyer (41:50):
Expect
Joe Aguilar (41:50):
That one, did you? No, I did not expect that one. I always say, knock on wood, knock on you. But I think our wood is solid because we look at the facts and circumstances. So each of our opinions are certainly rooted in the analytical, quantitative analysis, but it’s also, I can tell a storyline. So I get concerned if I’m being told something by my client and I’m looking at the provider and they’re not really aligning with their value. That being said to me, then I’m a little bit concerned it raises an eyebrow. Well, you
Conrad Meyer (42:29):
Knock on wood, let’s knock on wood for that one. Okay, yeah,
Joe Aguilar (42:31):
Absolutely.
Conrad Meyer (42:32):
I’ll do a follow-up absolutely. While I’m thinking about it. When I’m thinking about it. Okay, this is the second question.
Joe Aguilar (42:36):
Lemme see. I feel like I’m on rapid fire. You
Conrad Meyer (42:37):
Are on. This is a crossfire with Rory and I, so this is good. This is really good. So have you ever been called by a client or anyone on your team, but called by a client where you go in and they say, Hey, whatever the valuation is, and you get in there and you’re looking at it and you’re saying, oh boy, we need to do something here,
Joe Aguilar (42:58):
Meaning that the client is unhappy with what No,
Conrad Meyer (43:01):
No, no. The client is over overvaluing or the valuation is so off that you have to say, we have a problem, we need to dial it back.
Joe Aguilar (43:10):
Oh, yeah, yeah. It’s not a fun conversation. No. With the
Conrad Meyer (43:13):
CEO EO or Yeah,
Joe Aguilar (43:15):
Right. No, it’s not a fun conversation. How do you
Conrad Meyer (43:17):
Manage that? The personalities? You can’t tell those people. No, they don’t want to hear.
Joe Aguilar (43:22):
No. Yeah, yeah. No. Well, we do. I mean, I think that’s what we do, and I think it’s important. It’s a hard conversation. Yeah. I will tell, maybe I told this to Rory when he stopped by at the booth that we have a healthy no rate as well. I mean, that’s kind of what we say. It’s still low on the scheme of things because really hospitals are still a business and they need to figure out how to do this in a manner that’s sustainable. But there are situations where they need to just dial it back. But it’s not just, we just say, Hey, you need to dial it back. We will get into the same way we talked about hospital based arrangements. We’ll get into the detail and the metrics and say, Hey, and then the other things we’ll put on our Kevlar jacket and have that conversation with the physicians ourselves as well. Good luck. Well, I’ve,
Conrad Meyer (44:10):
That’s a hard conversation. I bet.
Joe Aguilar (44:12):
Yeah. I’ve got scars to prove it, but I think that that’s where our role is. In other words, the hospital wants to pay as much as they can within reason. The physicians want to get paid as much as they want, like anybody else. And so our role is to kind of figure out what that playing ground looks like. And so I will tell our clients and offer it up. Hey, I’m happy to talk with them. And I think that’s where, I mean, I’m not a physician, but I think that’s where sometimes the clinician helps a bit, so we can talk through it. And I’ve been lucky, Conrad, most of the physicians have been very
Conrad Meyer (44:48):
Reasonable.
Joe Aguilar (44:49):
Yeah, they’ve been receptive. They may not have agreed, but I think we could come to a,
Conrad Meyer (44:55):
Well, it’s good you’re sort of the third party because the distrust between hospital administration and physician has been around for decades. And so by having you come in, even if you’re hired by the hospital and having that data-driven discussion, because they’re data people themselves, they’re science and math oriented. And if you have that discussion, I think that would go over much better than having an administrator have that discussion.
Joe Aguilar (45:18):
Right, right. Well, what’s interesting too is that we value and we value agreements and agreement terms. So we have situations where you could be an orthopedist, let’s say in trauma, and you are taking call for the entire hospital every day for trauma cases, even though the panel for orthopedic care is being shared amongst 10 other physicians. So what does it happen on the ground is that basically on the day that you’re not taking call, you get a call from a community physician because it’s an acetabular fracture, it’s some complex fracture. And so then from the physician’s perspective, who’s talking about their comp, they’re saying, well, wait a second, I’m really on call 365 days out of the year, but I’m only getting paid for 40 days. And they’re true. It’s true. It’s legitimate. It’s legitimate. So then how do you fix that? Well, we can’t fix it by, I like to say that there’s buckets. When you think about all the different things that the physician does, it’s valued in different buckets. And I can’t make the bucket bigger because for call, I can only do what I can with regards to the services that they’re offering. But that’s when we have that conversation with the hospital, CEO, who’s upset and say, well, you know what? He’s providing calls so we can, why don’t we set that up and consider these things? So we peel back the onion and try to help. That’s good.
Rory Bellina (46:43):
Very good. One thing I wanted to ask you, and Conrad knows that I hate saying it, but we talked about it for probably two years and did different episodes on it, is the C word is covid from, we saw what happened from a compensation standpoint for providers and really from CMS and reimbursement, but can you explain what you saw as a valuation firm during covid? And then what are you seeing now? What’s changing? I mean, obviously you were contacted from providers during covid on compensation, but what did you do during then? And then now what’s swinging back another direction now?
Joe Aguilar (47:21):
Yeah, so covid was a unique year, obviously that’s an understatement. We did a lot of in the surge business, in other words, how do we cover the ICUs, the ERs and so forth on physician comp related material. We didn’t do a whole lot because of the waivers that were in place, especially if it was related to covid. But the afterwards, so the 20 21, 20 22, when you had transactions and you had COVID dollars in those transactions, you had to be kind of careful because the folks who sold during COVID 2020 typically had a very low ebitda. And so their multiples were very high. So if you just took the multiples from 2020 for instance, and you applied it to your 2021 transactions, you were seeing just overvaluing because the EBITDA were so low on during the COVID year, so you had to be careful. So thankfully, we’re not really seeing much of an impact anymore.
Rory Bellina (48:29):
Are you seeing a realignment of physician compensation or provider compensation now that we’re out of it and that things are going back to, or things have gone back to you, but essentially more of a normal of where you’re not needing that ER coverage and that ICU coverage like you were before, and there’s arguably more providers now back in the workplace.
Joe Aguilar (48:48):
Yeah, what’s interesting, yes. Yes. So I definitely think we’re getting back to normal in terms of compensation. What we are seeing though is hospitals asking for more of those surge rates. And for instance, in with the RSV and pediatric hospital care with RSV going up in these last couple months, we were asked to look at how do we pay for some of these surges that occur that really weren’t, and the RSV isn’t new, but it really wasn’t a topic until covid from that
Rory Bellina (49:20):
Standpoint. I didn’t know if you had experience where you had an increased in provider comp, but now it’s had to come down. And if hospitals had to justify that to their docs,
Joe Aguilar (49:30):
We haven’t. And it’s mixed in. There is another topic that is probably also another hour is what is
Conrad Meyer (49:39):
About an hour
Joe Aguilar (49:40):
Is the change in the fee schedule. So with the work RVU values and the e and m, so all that kind of muddied things a lot because you saw primary care physicians overnight, if you stayed on, if you moved, stayed on the same conversion factor, and you moved to the new fee schedule, keeping volumes the same. You saw 20, 25% increases in comp. And so all that kind of money, but it was a
Conrad Meyer (50:08):
False bottom because what they did was they raised the RVs, but they reimbursed at the same rate. So how do you tell a doc on an RVU production model to say, Hey, by the way, you’re going to get a 30% bump, but we’re not going to pay you.
Joe Aguilar (50:20):
And that’s, that’s crazy. No, that’s incredible. And so we counseled a lot of
Conrad Meyer (50:27):
Hospitals
Joe Aguilar (50:28):
Because we were having them look at that in the sense that they weren’t going to have the money to pay.
Conrad Meyer (50:34):
It was a terrible, terrible thing what CMMS did with that. And to me, it made no sense. I’m like, if you know everybody’s doing production comp, why would you even do it? Why would you even alter the rvu, the work RVs?
Joe Aguilar (50:43):
Right. Yeah. I think it was a long time coming and it just came at the wrong time. It didn’t, and considering covid and considering all the other things that were coming out of, I
Conrad Meyer (50:52):
Agree with you on the EBITDA return on the multiples during covid. I mean, it totally dipped because the trailing production in revenue was not there. No, not even close. And so I saw an article recently about, we’re going to get to private equity a little bit. Did you see an influx in covid of private equity sort of sweep up maybe a sweetheart deal because the EBITDA was so they could argue a lower EBITDA on a buyout because of covid. Did you see that? And where do you see that going in 2024?
Joe Aguilar (51:27):
Well, I definitely see it growing, I think 2021, I have another team that does a lot of the transaction work, but we definitely saw it in 2020, but in 2021 as well. And I think 21 was a big year. I can’t remember if it was 22.
Conrad Meyer (51:42):
Even with the T trache payments, it wasn’t
Joe Aguilar (51:44):
Enough. No. And I think that you’re going to continue seeing private equity continue to grow. I definitely think there’s a continued big interest, and it’s obviously changing in terms of the specialties that they’re focusing on. But I have a piece on private equity acquisitions in MGMA Connection this month and where basically what we’re saying is that it just depends on where the horizon is for those physicians that are in the private practice. So if a lot of the physicians who’ve held out up until this point, if they’re getting to the point where they’re in their twilight years of private equity, that’s the drive makes sense for them completely if they’re in the younger years. Well, some of the compensation arrangements that are available at the hospital or the health system level, which is very different than the private equity level, may be more attractive to that 30 something year old. But either way, I think private equity’s not going away.
Rory Bellina (52:47):
Think so. Do you still see that it’s focused heavily on your dermatology, radiology ortho, or do you see it shifting now to other industries going forward in 2024
Joe Aguilar (52:58):
ASCs, we saw probably cardiology started to wean down last year hitting all the specialties you mentioned definitely radiology and ortho, but I think right now there’s still a lot of work in that space.
Rory Bellina (53:14):
Okay,
Conrad Meyer (53:16):
Interesting. Well, I mean, I could tell you we could go on a hole. Every little thing that we have a rabbit hole on, whether it’s PE or whatever, we could do an hour on that. And I tell you, that’s why I love healthcare. I mean, I’ve been doing healthcare since, like you were saying in the early nineties, I was at HCA a, we’ve been doing MO days. So I mean, I love talking about this and I like seeing the trends, and it’s good to be able to spot the trends and being able to help providers work through
Joe Aguilar (53:47):
That.
Conrad Meyer (53:49):
I think you’re doing a great job. I mean, I’m very intrigued. I’m very happy that you came on the show today. Same
Joe Aguilar (53:54):
Here. Same here.
Rory Bellina (53:54):
Yeah, absolutely. So I mean, yeah, before we close, is there anything that you wanted to end with on where you see things going in 2024? I know we have an election at the end of the year. Is there anything that you wanted to lead into? Because we definitely want to have you back to talk
Joe Aguilar (54:07):
More. I definitely don’t want to comment on any elections. I’m not, no, we’re not going
Conrad Meyer (54:11):
To get a politic. We’re not going to get
Joe Aguilar (54:12):
There. But no, I mean, I think from a healthcare and valuation perspective, I think it, it’s complex. And I think that for health systems clients, I think really they’re looking for partners. And I think that’s a key in looking at how they handle and how they remain compliant because they have limited resources. And so we know the financial pressures that are out there. And so what we’re basically arguing is that not every valuation firm needs to be, or not every valuation. You need to spend that many resources to support, but you definitely need to be cautious about how you approach each of those arrangements.
Conrad Meyer (54:56):
Well, I want to thank you very much for taking the time in your busy schedule to come sit down and talk to us in our studio here. I think I’m agreeing with Rory, even if we do remote, I would love to have you back on some of these other topics and maybe have a panel discussion. If we could put someone together like that, I think that would be fantastic.
Joe Aguilar (55:12):
Absolutely.
Rory Bellina (55:14):
We really appreciate it. But if you want to give your contact information to our listeners and we’ll wrap it up. Yeah, go
Joe Aguilar (55:18):
Ahead. Sure, sure. Okay. Well, you can reach me at Joe Aguilar, that’s A-G-U-I-L-A-R@hmsvalue.com. Or you can reach me by phone at (678) 984-6435.
Conrad Meyer (55:38):
Fantastic. That’s great. Well, Joe, thank you so much for coming. Thank you on the show today. And everyone, thank you so much for listening in to another healthcare episode here at Health Law Talk at Chehardy Sherman Williams. Have a blessed day, and until the next time Take care.
Intro (55:51):
Thanks for listening to this episode of Health Law Talk, presented by Chehardy Sherman Williams. Please be sure to subscribe our channel. Make sure to give us that five star rating and share with your friends. Chehardy Sherman Williams is providing this podcast as a public service. This podcast is for educational purposes only. This podcast does not constitute legal advice, nor does this podcast establish an attorney client relationship. Reference to any specific product or entity does not count as an endorsement or recommendation by Chehardy Sherman Williams. The views expressed by guests on the show are their own, and their appearance does not imply an endorsement of them or their entity that they represent. Remember, please consult an attorney for your specific legal issues.